What is Immunotherapy?
The immune system plays an important role in keeping us healthy. For example, immune cells fight infections by recognizing that a virus or bacteria does not belong in our body and then destroys it. The immune system also destroys most cancer cells as they form. Unfortunately, some cancer cells figure out ways to “hide” from the immune system. By hiding from destruction by the immune system, these cancer cells have a chance to grow and spread to another part of the body.
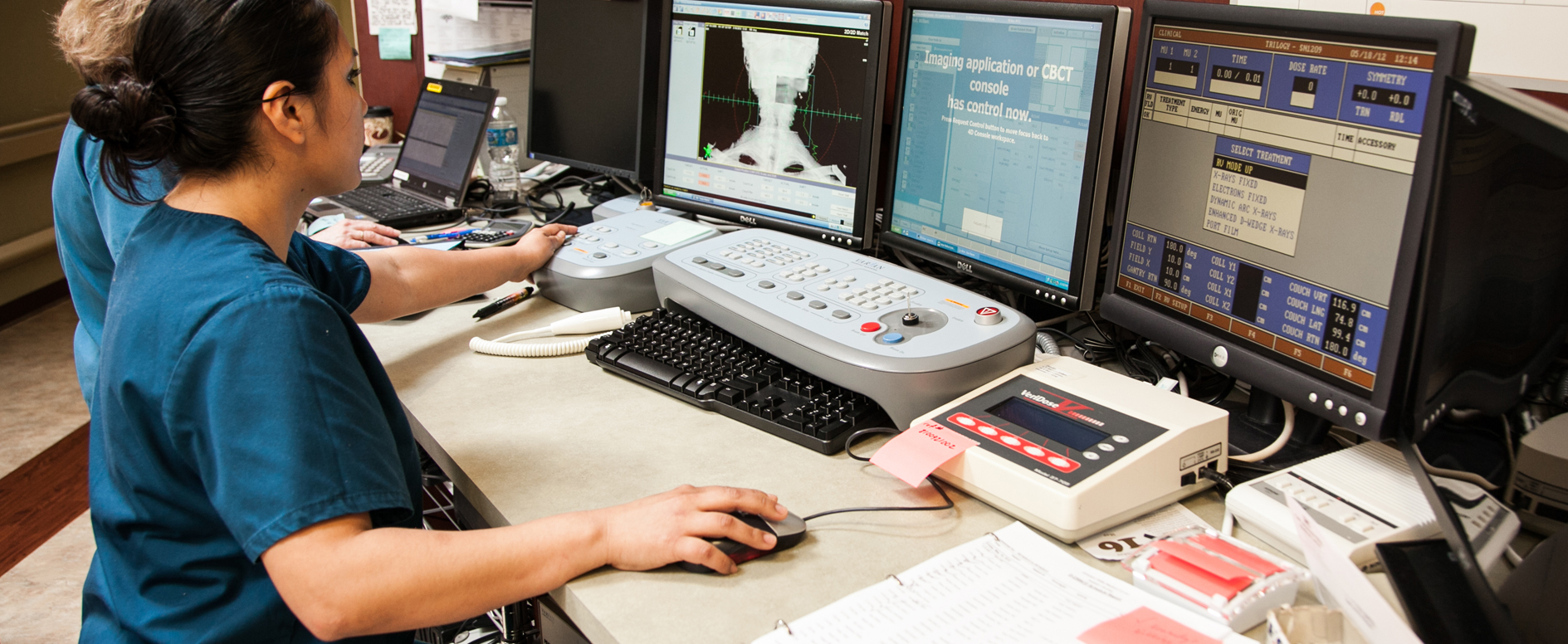
Immunotherapy is a type of drug or medication that can block the signals that cancer cells use to “hide” from our immune system. Blocking these signals allows the immune system to fight cancer in a very different way than other treatments like chemotherapy or radiation therapy, which directly damage cancer cells. There is still a lot to learn, though, about how to best use immunotherapy to fight cancer. While some cancers respond extremely well to immunotherapy, many still do not respond well. Most of the time, immunotherapy and radiation are used independently to treat the same cancers. Radiation therapy may help immunotherapy work better in some situations. This is a topic of active research at many cancer centers.
When are radiation and immunotherapy used together to treat cancer?
At this time, immunotherapy is most often used to treat cancer that has spread to other parts of the body. This is called metastatic cancer. Immunotherapy is also used along with surgery, radiation and chemotherapy to treat patients with cancer that has not yet spread.
Most patients with stage 3 non-small cell lung cancer now receive many months of immunotherapy after they complete their initial treatment with radiation and chemotherapy. Researchers have found that giving immunotherapy after radiation and chemotherapy increases the chances of long-term survival. It also reduces the chances of cancer coming back.
Many patients with esophagus cancer receive chemotherapy and radiation before having surgery. Unfortunately, some still have cancer after completing chemotherapy and radiation. Cancer that does not fully respond to chemotherapy and radiation can have higher chances of coming back after surgery. Researchers have found that additional treatment with immunotherapy after surgery in this setting increases the chances of surviving cancer. It also reduces the chances of cancer coming back.
Breast cancer is often treated with a combination of surgery, radiation and medications such as chemotherapy. Many patients with an aggressive form of breast cancer, called triple negative breast cancer or TNBC, receive chemotherapy before they have surgery to remove their breast cancer. While the chemotherapy can help shrink the cancer for surgery, doctors can also find out how well the cancer responds to chemotherapy. If the cancer responds well to treatment before surgery, it can mean the patient has a better chance of cure. However, not all patients with TNBC have a good response to chemotherapy. For this specific subtype of breast cancer, researchers have found that giving immunotherapy along with chemotherapy before surgery increases the number of patients whose cancer goes away completely. After surgery, some TNBC patients receive radiation. When immunotherapy is given, it might be continued after surgery and during radiation.
What type of side effects can occur?
Most patients do relatively well with immunotherapy from a side effect perspective. This type of treatment can sometimes cause a skin rash or flu-like symptoms. Flu-like symptoms can include tiredness, chills, weakness, dizziness, muscle or joint aches. Immunotherapy can also cause side effects in the digestive system. These side effects include diarrhea, nausea or vomiting. In rare cases, immunotherapy can cause severe inflammation of either the bowel (colitis) or lungs (pneumonitis). If this occurs, the medication may need to be stopped.
We are learning more about using radiation therapy together with immunotherapy. Each of these treatments can cause their own side effects. However, they likely can be used safely together in most cases. Radiation therapy can also create inflammation in the areas it is used. Because of this, careful attention should be paid to make sure that the more concerning inflammation in the colon or lungs does not occur if both treatments are used at the same time.
How might radiation and immunotherapy be used together in the future?
Many research studies are ongoing to determine if radiation and immunotherapy can be combined to further enhance the effects of each treatment. However, these approaches are not widely used yet as part of routine cancer treatment. One area of research is exploring whether radiation can be used in patients with metastatic cancer who have only a few visible areas of cancer. Some studies have shown that targeted radiation may prolong the time that cancer can be kept from growing or spread by immunotherapy. When cancer cells die from radiation, they can activate the immune system. This has led to studies asking whether radiation to one area of metastatic cancer can help cancer in another area respond better to immunotherapy. This has also led to studies asking whether immunotherapy given during or after radiation could improve the chances of getting rid of the cancer completely with radiation.
Questions?
Do you have questions about immunotherapy? Are you wondering if this type of treatment might be an option for you? If so, talk with your radiation doctor or medical oncology (chemotherapy) doctor. They can help you to learn more about this new category of treatment.